Achieve Financial Velocity
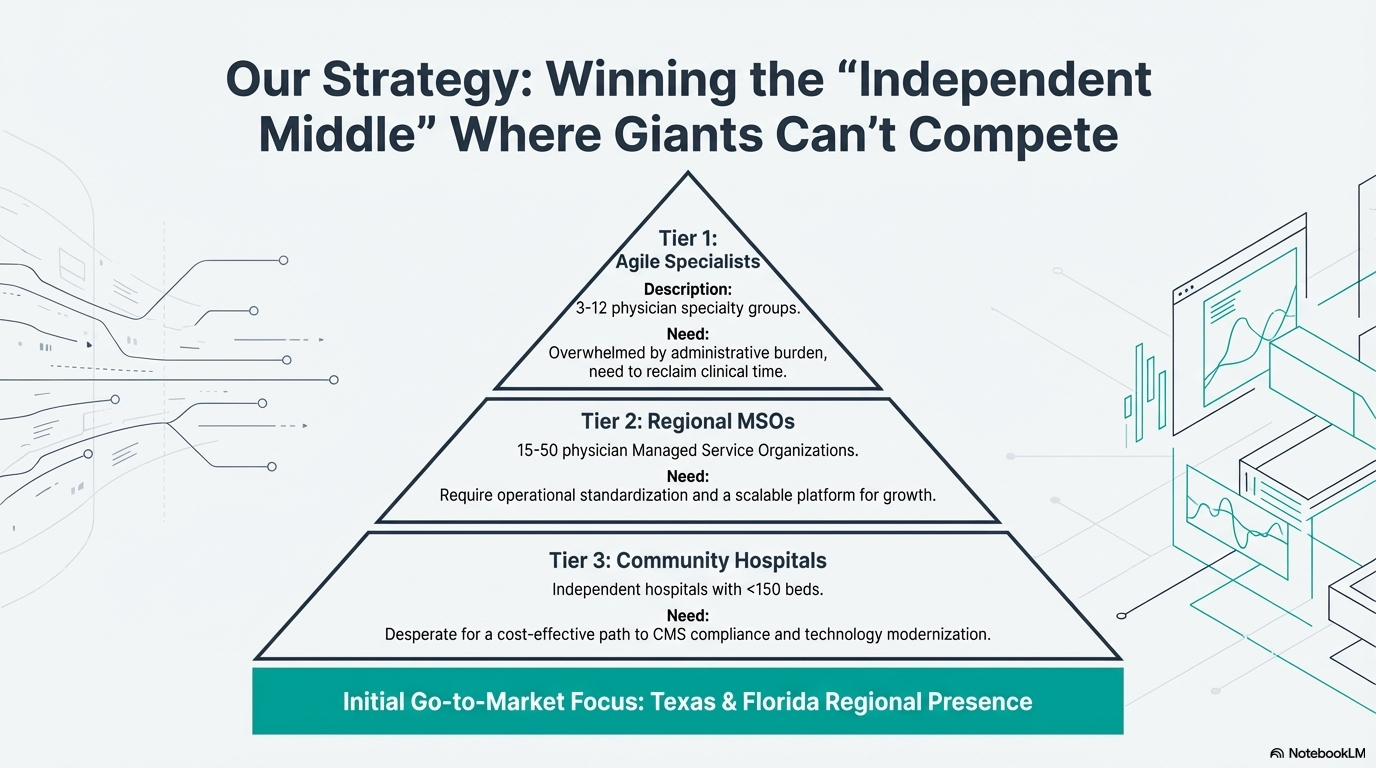
We provide the governance that unlocks trusted AI in healthcare. Connecting clinical truth to financial outcomes for independent providers, MSOs, and community hospitals.
We provide the governance that unlocks trusted AI in healthcare. Connecting clinical truth to financial outcomes for independent providers, MSOs, and community hospitals.
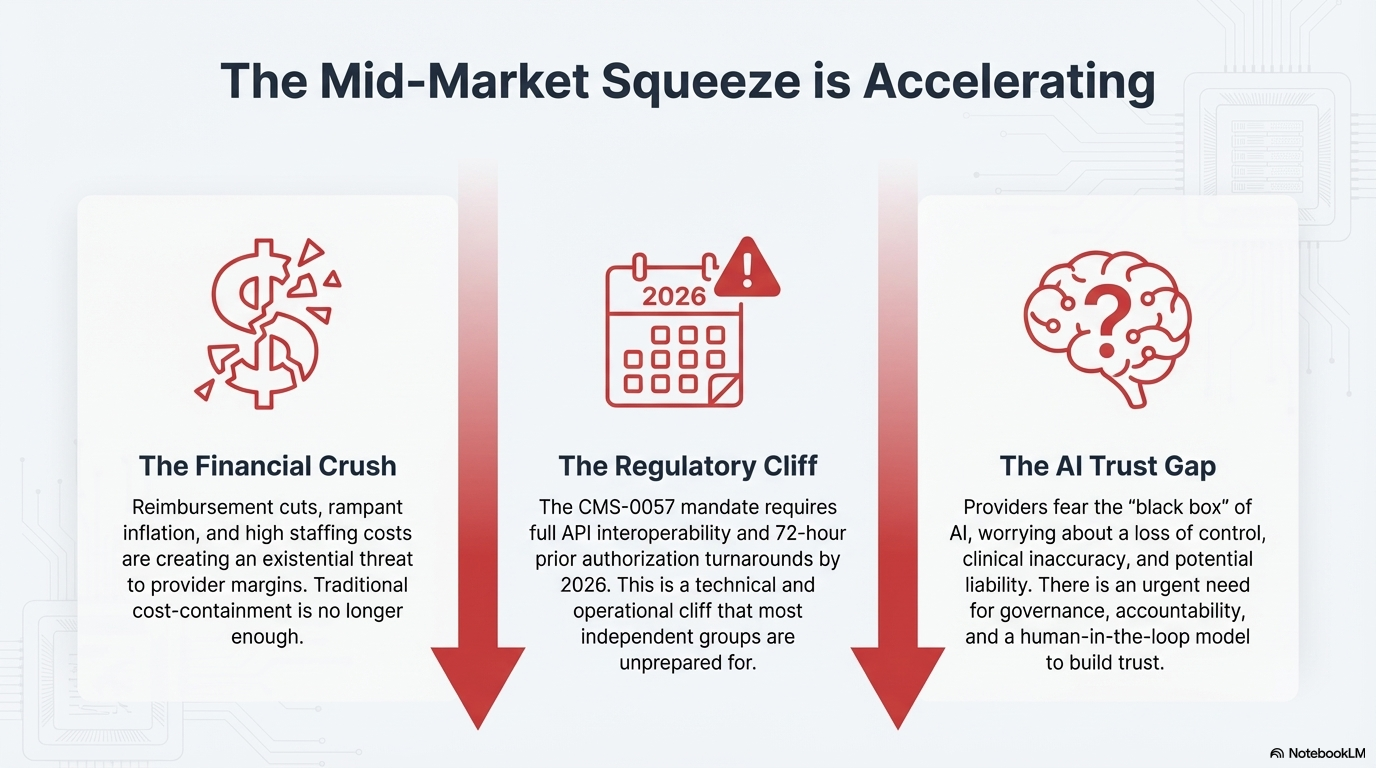
Pure AI is a powerful tool, but it's prone to hallucinations and errors. Our "Human-in-the-Loop" (HITL) model, staffed by TX/FL/Global domain experts, provides the crucial layer of review and accuracy that the market demands.
AI provides the speed; our experts ensure the truth.

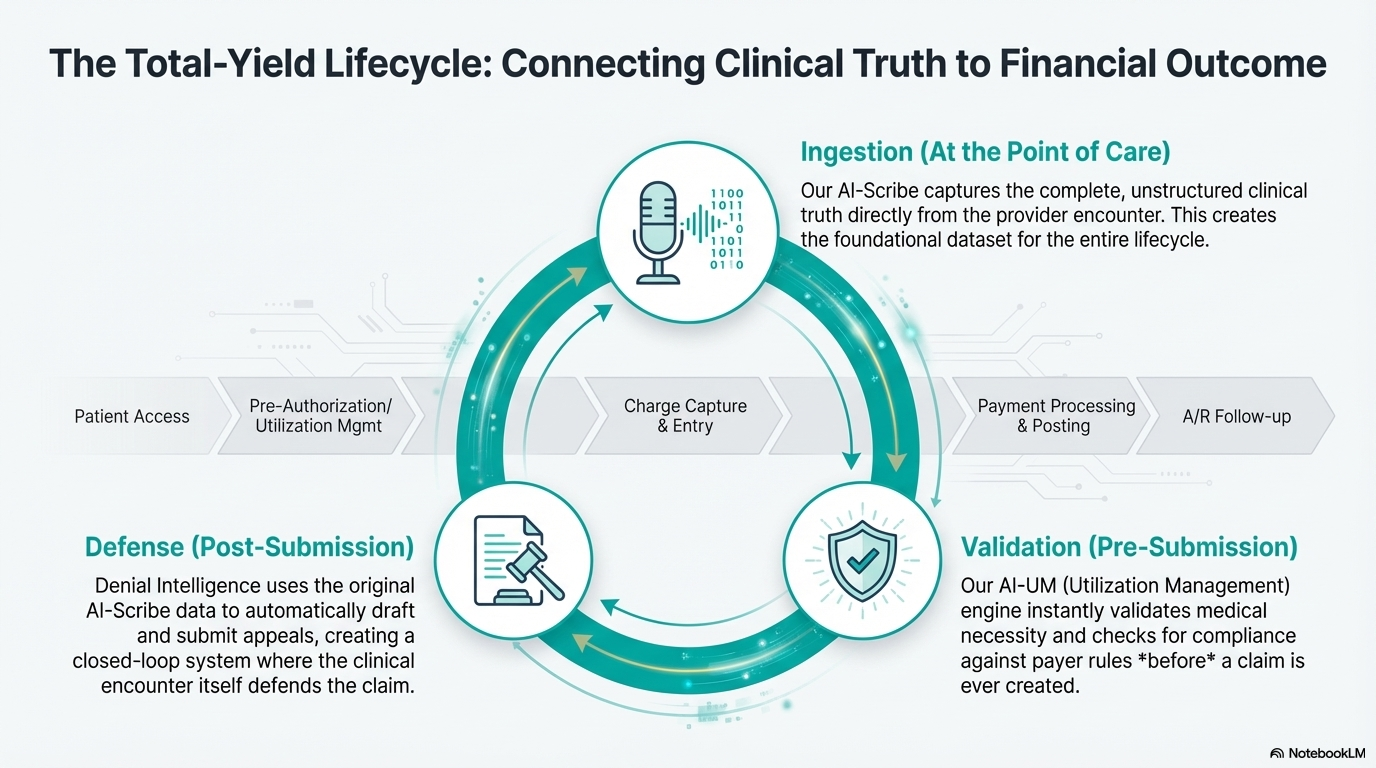
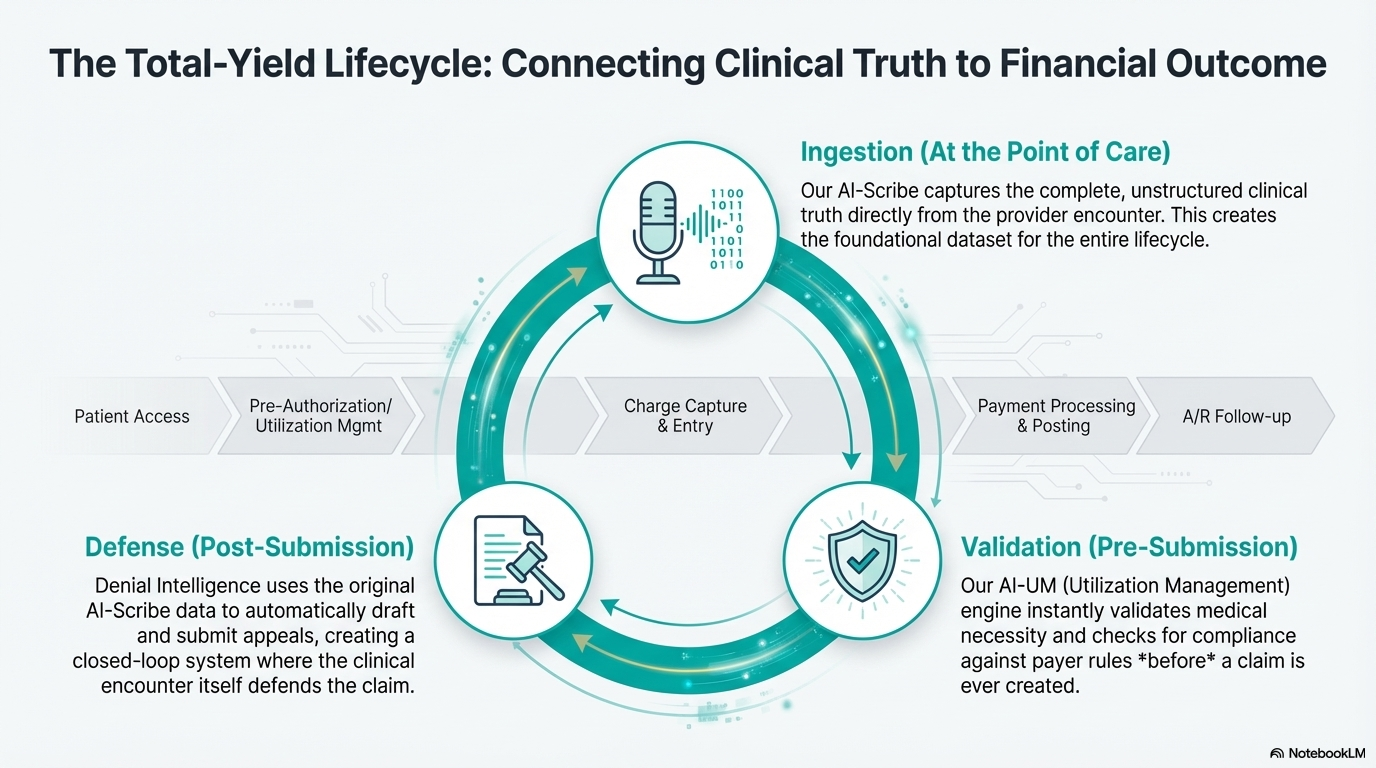
Connecting clinical truth to financial outcome across the entire revenue cycle.
At the Point of Care
AI-Scribe captures the complete clinical truth directly from the provider encounter. This creates the foundational dataset for the entire lifecycle.
Pre-Submission
Our AI-UM engine instantly validates medical necessity and checks for compliance against payer rules *before* a claim is ever created.
Post-Submission
Denial Intelligence uses the original clinical data to automatically draft and submit appeals, creating a closed-loop system where the encounter itself defends the claim.

We don't replace; we optimize. Talisman is the "AI-Brain" that connects to your existing systems of record. We ingest the clinical and financial data, orchestrate the complex workflows, and push clean, actionable results back into your native environment.
"In a six month period Talisman Solutions increased our Practice's income by over $100,000. Their innovative RCM services and patient Acquisition Services were a God send!"
"Since we switched our billing to Talisman, we have definitely seen an increase in our monthly income. They always follow up on outstanding claims and provide great communication."
"I have used Talisman Solutions for over a year. They are much better than my previous medical billing company. Talisman gives me personalized service which I really appreciate."
Let's discuss how Talisman can transform your revenue cycle with AI-powered solutions and expert accountability.